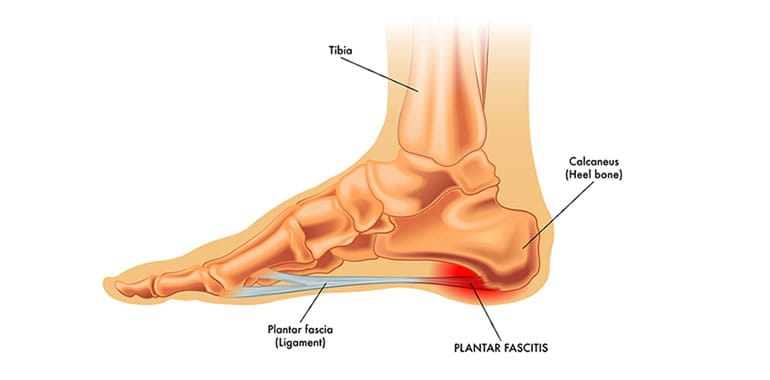
Plantar fasciitis, a condition characterized by inflammation of the thick band of tissue connecting your heel to the ball of your foot, is a common source of foot pain. While it can be frustrating to deal with, there are effective strategies for both treating and preventing this condition.

What is Plantar Fasciitis?
The term “plantar fasciitis” itself provides some clues. “Plantar” refers to the sole of your foot, and “Fascia” refers to a broad band of connective tissue. The term “itis” indicates inflammation.
Essentially that means plantar fasciitis is an inflammation of the plantar fascia, a strong, fibrous band of tissue that supports the arch of your foot. This ligament plays a vital role in absorbing shock and providing stability during walking, running, or any activities where you need to use your feet.
Common Causes Contribute to the Development of Plantar Fasciitis
To effectively address plantar fasciitis, it’s crucial to understand its underlying causes. Repetitive activities that place significant stress on the plantar fascia can contribute to its inflammation. This includes activities such as running, jumping, and prolonged standing.
Stiffness in the calf muscles and Achilles tendon can also increase tension on the plantar fascia. This tightness can pull on the heel bone, further irritating the ligament.
Abnormal foot biomechanics, such as flat feet or high arches, can disrupt the natural distribution of weight. This can lead to excessive strain on certain areas of the foot, including the plantar fascia.
With age, the plantar fascia can become less flexible and more prone to injury. This natural aging process can increase the risk of developing plantar fasciitis.
Obesity significantly increases the load on the feet, as the extra weight puts additional stress on the plantar fascia, making it more susceptible to inflammation.
Wearing ill-fitting shoes or those that lack adequate support can contribute to the development of plantar fasciitis. Shoes that don’t provide proper arch support or cushioning can misalign the foot and place undue stress on the plantar fascia.
The Primary Symptom of Plantar Fasciitis is Sharp Foot Pain
Particularly in the heel or the bottom of the foot. First thing in the morning, after resting overnight, the initial steps can be particularly painful. You may even experience pain after periods of inactivity. The pain may also worsen after sitting or standing for extended periods.
The good news is that plantar fasciitis can be effectively managed with a combination of approaches and a little help from your favorite physical therapist. While not a cure, certain home strategies can provide temporary relief and improve discomfort. This includes rest! Avoid activities that aggravate the pain and allow the plantar fascia to rest.
Ice applied to the affected area for 15-20 minutes at a time, several times a day, and you can also looks at doing some stretching exercises. Over-the-counter pain relievers like ibuprofen or naproxen can help reduce pain and inflammation, but it’s a good idea to speak to a doctor or pharmacist to get some advice on that.
Regular stretching can reduce tension in the plantar fascia
- Plantar Fascia Stretch: Gently pull your toes towards your shin, holding the stretch for 30 seconds. Repeat several times throughout the day.
- Calf Stretches: Perform both standing and seated calf stretches to improve flexibility in the calf muscles.
- Towel Scrunches: Place a towel on the floor and use your toes to scrunch it up, holding for a few seconds. Repeat several times.
- Arch Lifts: While seated or standing, try to lift the arch of your foot off the ground, keeping your heel and toes in contact with the surface.
Consider these Approaches for Sustained Relief and Prevention
Custom Orthotics – Custom-made orthotics provide personalized support for your feet, helping to distribute weight more evenly and reduce stress on the plantar fascia. At PRO Therapy, we offer custom orthotics from Foot Levelers, designed to address your unique foot structure and biomechanics.
Physical Therapy for Plantar Fasciitis – A physical therapist can assess your condition, identify the underlying causes, and create a personalized treatment plan. This may include Manual therapy techniques such as massage and soft tissue mobilization to reduce pain and improve flexibility.
Therapeutic exercises designed to strengthen the muscles that support the foot and ankle, improve flexibility, and enhance balance. While dry needling – A technique that involves inserting thin needles into specific points in the muscle, is meant to release tension and reduce pain.
Physical Therapy for Plantar Fasciitis at PRO Therapy
At PRO Therapy, we take a comprehensive approach to treating plantar fasciitis:
- Thorough Assessment: We begin with a detailed evaluation to understand the root causes of your pain, including your medical history, lifestyle factors, and foot biomechanics.
- Personalized Treatment Plans: We create customized treatment plans that address your specific needs and goals.
- Focus on Long-Term Relief: Our aim is not just to alleviate pain but also to prevent future occurrences by addressing the underlying biomechanical issues.
- Education and Guidance: We provide you with valuable information and guidance on how to manage your condition, including proper footwear choices, stretching exercises, and lifestyle modifications.
Don’t Let Plantar Fasciitis Limit You
If you’re struggling with plantar fasciitis, don’t hesitate to seek professional help. At PRO Therapy, we can help you find relief from foot pain and get back to doing the things you love.
- Just Been in a Car Accident? Here’s What You Need to Know About Recovery - June 27, 2025
- How to Avoid Low Back Pain While Golfing - June 23, 2025
- Post-Accident Recovery: The Role of Shockwave Therapy - May 12, 2025